

Engage with us
Let us know what you’re interested in
and we will be happy to help
The platform seamlessely integrates with payer systems, providing a secure environment for communication and data transactions between payers and providers. Whether it's basic functions like identifying eligible members or advanced analytics on clinical data, the platform serves as a comprehensive sollution for cashless transactions.
The arrangement empowers consistent cooperation between the Emergency clinics and Payers across every one of the phases of a protection guarantee. Its handling motor completely digitizes claims handling and empowers continuous following of guarantee settlement status.
Read More
Workflow processes supporting hospital and insurance companies to control, track and manage in-patient insurance workflows on a single platform from admission to final settlements.
Hospitals can configure records of co-operations like Doctors, Health checks, and IP packages which can be used by the payers to provide information to their members and enhance the experience

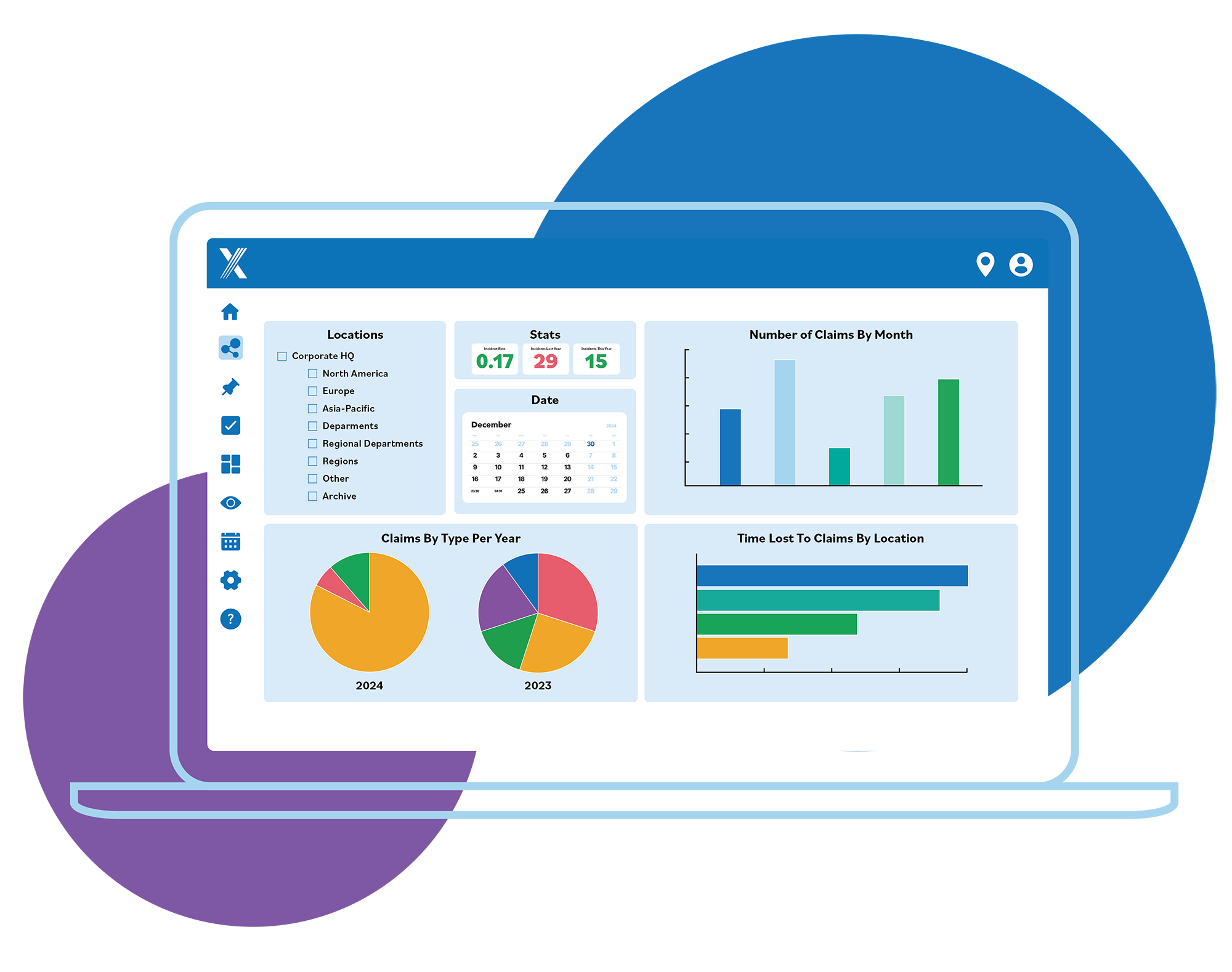
Hospital and payer finance teams have complete visibility on status of insurance claims and can use insights to manage receivable and payables
It has other regulatory friendly features such as standard nomenclatures for Hospitals (based on ROHINI IDs), ailments (ICD 10) and procedures (PCS) which promotes standardisation and supports data comparability and analysis.
